Our mood is an emotional state, which colours the way we view life. Most of us have experienced transient lower-than-usual moods. We quickly readjust and function at our previous emotional level. This natural ebb and flow of emotions congruent with our experiences sometimes is the basis of depression being misunderstood and patients being mislabelled as weak, lazy and inability to ‘walk it off’.
To distinguish a ‘down spell’ from a depressive episode or a disorder we use the criteria of time. The individual must have felt bad most of the day, almost every day, for at least 2 weeks to meet the requirements for a major depressive episode. If the person has experienced 2 or more episodes or symptoms persist for 2 months, Major Depressive order will be considered as a diagnosis. Note that the persistence of low mood is linked to a period of time that displays the required number of symptoms.
Depression can also vary in severity but common signs include a wide range of emotional, cognitive, and physical symptoms that can interfere with daily life. Emotionally, individuals may experience persistent sadness, hopelessness, or feelings of worthlessness. They may also lose interest or pleasure in activities they once enjoyed. Depression can lead to difficulty concentrating, indecisiveness, and intrusive negative thoughts, sometimes including thoughts of self-harm or suicide. Physically, symptoms may include fatigue, changes in sleep patterns (insomnia or excessive sleeping), appetite fluctuations (weight loss or gain), and unexplained aches or pains. These symptoms can vary in severity and duration, significantly impacting a person’s overall functioning and well-being.
There are numerous explanations to account for depression. However, research consistently points to a complicated interaction between biological, psychological, social and sociocultural factors.
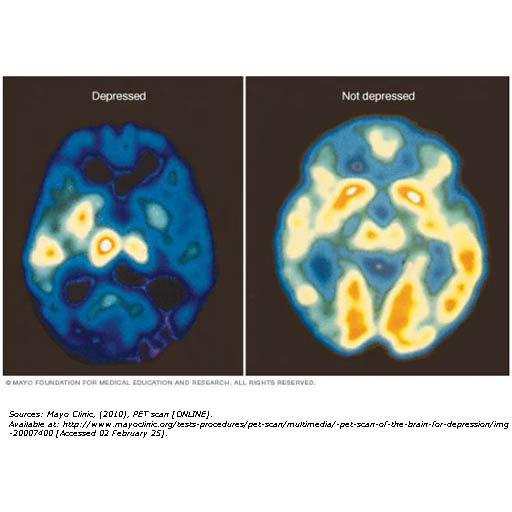
Depression can be influenced by various biological factors, including brain chemistry imbalances, genetics, and hormonal changes. Neurotransmitters such as serotonin, dopamine, and norepinephrine play a crucial role in mood regulation, and an imbalance in these chemicals can contribute to depressive symptoms.
Additionally, genetics can increase the likelihood of developing depression, as individuals with a family history of the condition may have a higher risk. Hormonal fluctuations, such as those occurring during pregnancy, postpartum, menopause, or due to thyroid disorders, can also play a significant role in triggering or exacerbating depression.
Psychological factors include negative thought patterns, past trauma, and certain personality traits. Persistent negative thinking, low self-esteem, and cognitive distortions, such as catastrophising or self-blame, can contribute to the development and maintenance of depressive symptoms.
Additionally, traumatic experiences in early life, such as childhood abuse, neglect, or the loss of a parent, can increase vulnerability to depression later in life. Personality traits like perfectionism, excessive self-criticism, or a strong dependence on others for validation may also heighten the risk, making individuals more prone to experiencing depressive episodes.
Social and environmental factors, particularly chronic stress, social isolation, and major life changes. Long-term exposure to stressors such as financial difficulties, job insecurity, or relationship problems can overwhelm an individual’s coping mechanisms, increasing the risk of depression. Additionally, a lack of social support and meaningful relationships can lead to loneliness, further exacerbating feelings of sadness and hopelessness. Even seemingly positive life changes, such as marriage or starting a new job, can be stressful and trigger depressive symptoms in some individuals, highlighting the complex relationship between external circumstances and mental health.
Medical conditions and lifestyle factors can play a significant role in the development and persistence of depression. Chronic illnesses such as diabetes, heart disease, or chronic pain can contribute to depressive symptoms by affecting overall well-being and quality of life. Additionally, substance use, including alcohol or drug abuse, can both trigger and worsen depression by altering brain chemistry and impairing judgment. Poor sleep and an unhealthy diet further exacerbate the issue, as sleep deprivation and nutritional deficiencies can negatively impact mood, energy levels, and cognitive function, making it harder to cope with daily challenges.
There are many options available to assist with the treatment of depression. Behavioural activation therapy, dialectical behavioural therapy, cognitive-behavioural therapy, and interpersonal psychotherapy have received extensive research support as effective treatments for depression; mindfulness-based cognitive therapy has also shown promising results. Biomedical treatments include light therapy and electrical stimulation of the brain. Antidepressant medications are frequently used to treat depression; they are most effective with severe depression but produce only temporary effects. Psychotherapy is more likely to prevent the return of depressive symptoms.
Several factors influence prognosis in mental health conditions. Early intervention typically leads to better outcomes, as seeking treatment promptly can prevent symptoms from worsening. Adherence to treatment, including therapy, medication, and lifestyle recommendations, plays a crucial role in recovery, with those who follow their treatment plans generally improving faster. A strong support system, including social connections and a healthy environment, further enhances prognosis. However, co-occurring conditions such as anxiety, substance use, or other medical issues can complicate recovery. Additionally, individuals with a history of recurrent depression are at higher risk for future episodes, but with preventive care, these episodes can be effectively managed.